Post-Surgical Physical Therapy (Rehabilitation)
Today’s healthcare consumer has more choice than ever, with a vast assortment of healthcare providers and specialists to serve your specific needs. Physical therapy was born of the medical profession more than a century ago and originally developed to rehabilitate those suffering disability following surgery or trauma. Physical Therapy is a service that by law can be provided only by a board certified and licensed Physical Therapist. The profession of physical therapy has evolved significantly over the past few decades, with physical therapists graduating today requiring a doctorate degree in Physical Therapy from an accredited university. As part of the medical community physical therapists utilize evidence-based practice to address your needs as efficiently and effectively as possible.
Following surgery, specific protocols developed by physical therapists in collaboration with the surgeon are followed. These protocols determine important milestones and timelines related to the progression of your rehabilitation. It is imperative that your specific protocol is observed to avoid premature stress on still healing tissues and protect the surgical site.
Treatments are also tailored within the protocol to your specific issues as assessed in examination and may include manual therapy techniques such as spinal, peripheral joint and soft tissue mobilization. Treatment may also involve modalities such as specific exercise, equipment and training/education depending on your situation.
Treatments used by physical therapist have undergone strenuous review through research to establish effectiveness. This review is part of Evidence Based Practice, the foundation of the physical therapy profession.

Do All Physical Therapists Treat Orthopedic Surgery?
Although all physical therapists are prepared through education and experience to treat people who have an orthopedic surgery, you may want to consider a specialist. The American Board of Physical Therapy Specialties has established a rigorous method to certify physical therapists that have unique experience, education or advanced knowledge in specific areas. An Orthopedic Certified Specialist (OCS) is a physical therapist that has an extensive history of experience and has completed a demanding board examination and are best equipped to provide care and guidance prior to or following an orthopedic surgery. In Utah,only 4% of physical therapists have this sanctioned professional designation. Active Lifestyles Physical Therapy is home to leading therapists specialized to best guide and serve you.

Physical Therapy Before & After Surgery
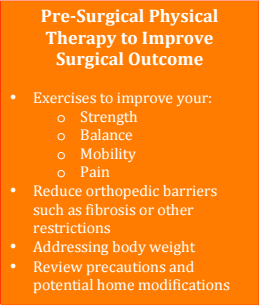
Before Your Surgery: "Pre-hab"
The better your health prior to surgery, the better your results will be especially in the short term. Before surgery overall health, tissue quality, strength and balance can all impact your results and speed of recovery. Therefore it is common practice to visit with a physical therapist to address issues related to function several weeks or months ahead of your planned surgery.
If you are a smoker it is highly recommended that you quit smoking to improve your healing times, reduce your pain and improve your rehabilitation results. If you are overweight, increase focus on weight loss prior to surgery. Losing excess body weight may also help you recover more quickly. Good nutrition and regular exercise (3 or more days/week) are also important for your fast recovery following surgery. It is best to continue with or begin an exercise regiment several months ahead of your joint replacement surgery. Your physical therapist is the most qualified medical professional to assist you in developing a strategy tailored to your needs.
Due to the vast and varying types of orthopedic surgeries the following material on this page is limited to the three most common arthroplasty procedures performed in the United States. For more information regarding other conditions, please explore the remainder of our website.
Total Joint Replacement (Arthroplasty)
The decision to undergo a joint replacement should not be taken lightly and be made in consultation with your orthopedic surgeon and your physical therapist. Following surgery the healing process and return to function can take several months. Repairing the human body is unlike repairing a machine or appliance; unfortunately it is not simply replacing damaged parts. Joint replacement surgery requires tissue healing over a predictable course of time and rehabilitation to regain optimal function.
Your physical therapist is the most knowledgeable and best-equipped healthcare professional to guide your return to optimal function following a joint replacement surgery.
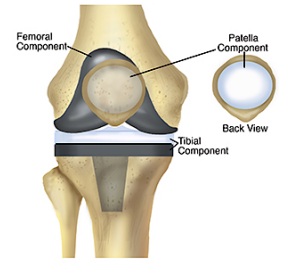
Total Knee Replacement / Arthroplasty (TKR/TKA)
The knee is the most commonly replaced joint in the body, with over 600,000 knee replacement surgeries performed in the United States annually and that number is expected to rise to 3 million by 2030. Total Knee Replacement (TKA) or Arthroplasty (arthro = Joint, plasty = repair) is a surgical procedure to resolve otherwise irreparable knee joint damage due to disease, osteoarthritis, rheumatoid arthritis or fracture.
A total knee arthroplasty (TKA) involves removing the ends of the bones that form the knee joint and replacing them with artificial parts. Replacement parts consist of a metal cap placed on the end of the thigh bone (femur) and a plastic cap placed on the top of the shinbone (tibia). Sometimes, a plastic insert is used to replace the undersurface of the kneecap (patella).
Total Hip Replacement / Arthroplasty (THR/THA)
Total Hip Replacement (THA) or Arthroplasty (arthro = Joint, plasty = repair) is a surgical procedure to resolve otherwise irreparable hip joint damage due to disease, osteoarthritis, rheumatoid arthritis or fracture. The hip is the second most commonly replaced joint in the body, though with the number and rate total hip replacements skyrocketing over the past decade. According to the CDC, from 2000 to 2010 the quantity of THA’s performed in the United States jumped from 138,700 to 310,800, or 257 per 100,000 people age 45 and over.
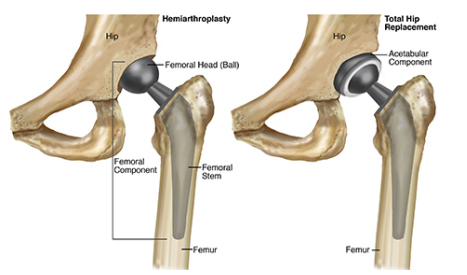
A total hip arthroplasty (THA) involves removing the end of the thigh bone (femur) and the acetabulum socket portion of the pelvis (acetabulum) that form the hip joint and replacing them with artificial parts. Replacement parts consist of a metal shaft and hemispheric ball placed on the end of the femur and an artificial surface placed in the acetabulum.
A hemiarthroplasty is performed when there is damage only to the femoral portion of the hip joint. With hemiarthroplasty, or partial hip replacement, only the ball is replaced. This is mostly performed in patients who are more fragile, elderly or with poor capacity to heal. This approach is also often used for fractures involving the ball or the upper shaft portion (neck) of the femur.
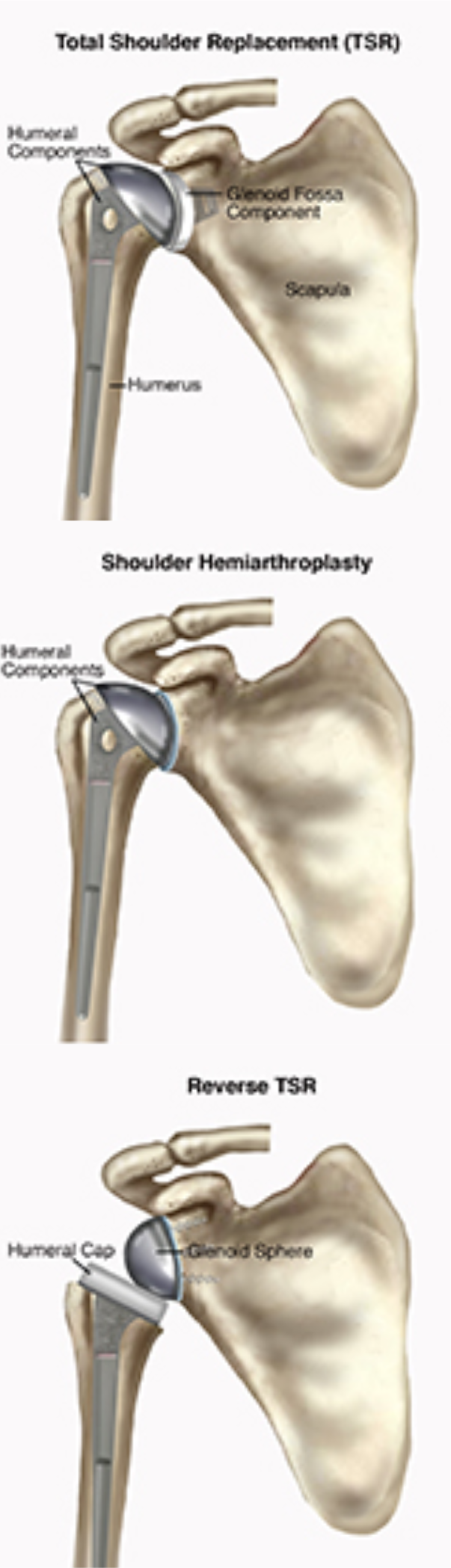
Total Shoulder Replacement / Arthroplasty (TSR/TSA)
A Total Shoulder Replacement or Arthroplasty (TSA) (arthro = Joint, plasty = repair), is not as common as knee or hip replacement surgery though it is estimated that 53,000 people in the United States have shoulder replacement surgery each year. A TSA is a surgical procedure to replace the end of the upper arm bone (humerus) and the shoulder blade (scapula) portion of the shoulder joint. A TSA surgery involves replacing the top of the humerus (head of the humerus) with a metal ball. The socket portion of the joint is known as the glenoid fossa of the scapula and is replaced by a shallow artificial socket. A Reverse Total Shoulder Arthroplasty is a similar procedure though the replacement components are reversed, with a shallow socket placed on top of the humerus and a metal ball on the scapula portion of the joint. This procedure is often used when there is irreparable damage to the rotor cuff muscles allowing the deltoid to partly take over function of the rotator cuff muscles.
Immediately Following Your Surgery
After a Total Joint Arthroplasty, you likely will stay in the hospital 2 or 3 days following your surgery. If you have other medical conditions, such as heart disease or diabetes, your hospital stay may extend 1 to 3 additional days. The early phase of rehabilitation is focused on controlling swelling and pain, though early work on range of motion is often critical. Most cases of Total Joint Arthroplasty are allowed to weight bear immediately or shortly after the surgery. Depending on multiple factors such as your health, mobility and home situation, a brief stay in a short-term rehabilitation inpatient facility may also be recommended by your surgeon.
A protocol developed by your surgeon in cooperation with your physical therapist is followed to guide rehabilitation following your orthopedic surgery. Protocols help establish a timeline for your recovery and regaining milestones of function. Post-operative protocols also highlight precautions and limitations related to your specific procedure in order to protect the surgical site and optimize your recovery.
Components of function are addressed during your rehabilitation. These components include controlling swelling and pain, range of motion, strength, body awareness/proprioception, balance and activity specific training. With your personal goals in mind, your physical therapist will develop an effective plan for optimal return to the activities
References & Resources:
The More You Know:
The following articles provide some of the best scientific evidence about physical therapist treatment of Total Joint Replacement / Arthroplasty surgery. The articles report recent research and give an overview of the standards of practice for treatment both in the United States and internationally. The article titles are linked either to a PubMed* abstract (summary) of the article or to free access of the entire article, so that you can read it or print out a copy to bring with you when you see your healthcare provider.
*PubMed is a free online resource developed by the National Center for Biotechnology Information (NCBI). PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Total Knee Arthroplasty:
Piva SR, Gil AB, Almeida GJ, et al. A balance exercise program appears to improve function for patients with total knee arthroplasty: a randomized clinical trial. Phys Ther. 2010;90:880–894. Free Article.
Piva SR, Teixeira PE, Almeida GJ, et al. Contribution of hip abductor strength to physical function in patients with total knee arthroplasty. Phys Ther. 2011;91:225–233. Free Article.
Moffet H, Collet JP, Shapiro SH, et al. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil. 2004;85:546–556. Free Article.
Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomised controlled trials. BMJ. 2007;335:812. Free Article.
Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Ortho Sports Phys Ther. 2010;40:559–567. Article Summary on PubMed.
Walls RJ, McHugh G, O’Gorman DJ, et al. Effects of preoperative neuromuscular electrical stimulation on quadriceps strength and functional recovery in total knee arthroplasty: a pilot study. BMC Musculoskelet Disord. 2010;11:119. Free Article.
Topp R, Swank AM, Quesada PM, et al. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM R. 2009;1:729–735. Article Summary on PubMed.
Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee [erratum in: N Engl J Med. 2009;361:2004]. N Engl J Med. 2008;359:1097–1107. Free Article.
Deyle GD, Henderson NE, Matekel RL, et al. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2000;132:173–81. Free Article.
Dowsey MM, Liew D, Choong PF. The economic burden of obesity in primary total knee arthroplasty. Arthritis Care Res (Hoboken). 2011 July 26 [Epub ahead of print]. Article Summary on PubMed.
Total Hip Arthroplasty:
CDC National Center for Health Statistics: Hip Replacements from 2000 – 2010 Report: https://www.cdc.gov/nchs/data/databriefs/db186.htm
Nanaku M, Tsuboyama T, Akiyama H, et al. Preoperative prediction of ambulatory status at 6 months after total hip arthroplasty. Phys Ther. 2013;93:88-93. Article Summary on PubMed.
Slaven EJ. Prediction of functional outcome at six months following total hip arthroplasty. Phys Ther. 2012;92:1386-1394. Free Article.
Vissers MM, Bussmann JB, Verhaar JA. Recovery of physical functioning after total hip arthroplasty: systematic review and meta-analysis of the literature. Phys Ther. 2011;91:615-629. Free Article.
Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits—hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from
the orthopedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39(4):A1-A25. Free Article.
Total Shoulder Arthroplasty:
ScienceDaily. Published July 13, 2009. Accessed February 11, 2015 Golant A, Christoforou D, Zuckerman JD, Kwon YW. Return to sports after shoulder arthroplasty: a survey of surgeons' preferences. J Shoulder Elbow Surg. 2012;21(4):554–560. Article Summary in PubMed.
Schumann K, Flury MP, Schwyzer HK, Simmen BR, Drerup S, Goldhahn J. Sports activity after anatomical total shoulder arthroplasty. Am J Sports Med. 2010;38(10):2097–2105. Article Summary in PubMed.
Boardman ND III, Cofield RH, Bengtson KA, Little R, Jones MC, Rowland CM. Rehabilitation after total shoulder arthroplasty. J Arthroplasty. 2001;16(4):483–486. Article Summary in PubMed.
Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603–616. Article Summary in PubMed.
History of Physical Therapy Education Terlouw TJA. Roots of physical medicine, physical therapy, and mechanotherapy in the Netherlands in the 19th century: A disputed area within the healthcare domain. J Manual Manipulative Ther 2007;15:E23–E41
Excerpts from Dr. Moffat’s Presidential Address at Physical Therapy ’96: Scientific Meeting and
Exposition of the American Physical Therapy Association; Minneapolis, Minn; June 14, 1996.
2017 American Academy of Orthopaedic Surgeons. http://www.anationinmotion.org/value/knee/
